Aortic valve stenosis
What is severe aortic valve stenosis?
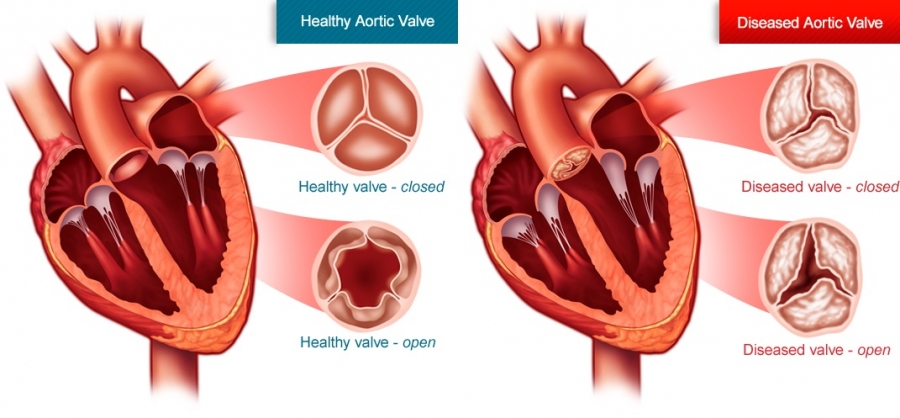
Aortic valve disease prevents the flow of blood from the left ventricle to the aorta and the rest of the body. These diseases are classified as congenital (the person was born with them) or acquired. The aortic valve may be narrowed, resulting in reduced blood flow to the aorta, or incompetent, resulting in backflow of blood into the left ventricle. Severe aortic valve stenosis occurs when the aortic valve cannot open properly and leads to hypertrophy of the heart muscle to push blood into the circulation which may over time lead to heart failure. Epidemiological studies have shown that the incidence of aortic stenosis increases with age. Over the age of 75, one in seven has moderate or severe aortic stenosis.
Causes and symptoms of aortic valve stenosis
Causes of stenosis can be:
- Congenital heart disease. The aortic valve consists of three triangular folds (cusps). There are children who are born with a single cusp, others with a two-cuspor even a four-cusp aortic valve. In adulthood, the valve may narrow or leak blood and need repair or replacement. For this reason, there should be a regular evaluation by a cardiologist.
- Calcification of the valve. Over the course of age, the valves of the heart can become calcified, a deposit of calcium on the valve or on its annulus (degenerative stenosis). In some patients, especially those with congenital heart disease, calcium deposition hardens the valve cusps.
- History of rheumatic fever at an early age, congenital valve abnormality, previous chest radiation, medications, rare metabolic or autoimmune diseases.
Risk Factors
Aortic valve stenosis cannot be predicted. Here are some risk factors that contribute to its occurrence:
- Bicuspid aortic valve.
- Age.
- Appearance of rheumatic fever.
- Chronic renal failure.
- High blood pressure, high cholesterol, type 2 diabetes and smoking.
Symptoms
The symptoms of severe aortic stenosis are related to the inability of the heart to supply blood to the coronary vessels and circulation, especially in cases of increased demands. Symptoms such as:
- Angina (chest pain) or tightness in the chest.
- Dizziness or fainting (fainting episodes).
- Shortness of breath, fatigue, periodically or during effort.
- Arrhythmia.
Aortic valve stenosis is a progressive and life-threatening disease. Once symptoms of heart failure (dyspnea), angina or syncope appear, life expectancy drops dramatically!
Ways to treat aortic valve stenosis
Appropriate medication helps reduce the intensity of symptoms but does not cure the problem. Effective treatment of severely narrowed aortic valve is done surgically either by repairing or replacing the valve.
1. Surgical treatment
Aortic valve replacement surgery is currently the treatment of choice for treating symptomatic aortic stenosis.
- Aortic valve replacement.
During the operation, the surgeon removes the narrowed valve and replaces it with a mechanical or biological valve. Mechanical valves have a long durability, but their use requires that the patient take anticoagulant drugs for life. Biological valves can be porcine, bovine or human and have a limited lifespan but do not require anticoagulation.
- Surgical correction of aortic valve stenosis.
In some cases, surgical aortic valve repair is indicated in comparison to balloon valvuloplasty, such as in infant cases where the valve cusps are united. The surgeon corrects the valve, reduces the narrowing and improves blood circulation.
2. Percutaneous transcatheter implantation(replacement) of the aortic valve (TAVI or TAVR).
In some patients, because of age or coexistent medical conditions, there is a high risk for surgical treatment of aortic stenosis. These patients can be treated with an alternative, percutaneous aortic valve implantation (replacement) (TAVI or TAVR).
Since the beginning of the 2010s, a new method of aortic valve implantation without the need for surgical intervention has been successfully tested. This is the so-called TAVI (or TAVR) intervention which is performed percutaneously by interventional cardiologists with a procedure similar to that of simple coronary angiography.
In percutaneous aortic valve replacement, the new biological valve is placed in the positionof the old with the aid of a catheter through either the femoral artery or the subclavian artery. The aortic valve is made of biological material (usually bovine or porcinepericardium), attached to a metallic stent. During aortic valve implantation the stent is deployed in the aortic wall between the heart and the aorta. The new valve, fixed on the stent, is placed over the old one, which is compressed, allowing the normal passage of blood from the heart to the rest of the circulation.
Before deciding whether a patient is suitable for percutaneous aortic stenosis treatment, some tests are necessary, which are carried out with a 24-hour admission and hospital stay.
These are:
- Electrocardiogram.
- Blood test.
- Ultrasound (Triplex) of the heart.
- Coronary angiography (Imaging of the arteries of the heart).
- CT angiography of the aorta and peripheral vessels.
These tests are prerequisites for the intervention because they assess the overall risk of the patient and provide important anatomic information for the planning of the interventional procedure. In this way, all the data are provided to the Interventional Cardiologists - Cardiac Surgeons for the indication of the intervention, but also for the kind of valve and the access to place the valve.
The operation is usually performed in the Catheterization Laboratory.
The exposure to radiation is less than twenty minutes, while the total duration of the operation is one to two hours. When the access site for the intervention is the femoral artery, only light sedation (no general anesthesia) is usually required. Initially, the old valve is expanded with a balloon (valvuloplasty) and in a second phase, through a larger catheter, the prosthetic valve is implanted under fluoroscopy.
Percutaneous placement of the aortic valve has clearly lower risks than the classic surgical treatment of aortic stenosis. For this reason, after all, it is the treatment of choice in patients with a high surgical risk. In fact, as the technique of percutaneous aortic valve implantation improves, this procedure has been deemed equivalent to surgical replacement even in patients with lower surgical risk.
There are some risks during the operation, some more and others less serious. In any case, the risk of death, cardiogenic shock, stroke is lower than with surgical treatment, while the only complications that occur more often are the need for permanent pacemaker implantation and vascular complications.
With the advances of technology and the accumulation of experience, the above disadvantages have been drastically reduced, and the method haslimited the need for surgical treatment of aortic stenosis, just as coronary angioplasty has significantly reduced the need for coronary bypass surgery (by-pass).
After the aortic valve implantation, the hospital stay lasts 3-4 days. The initial stay is in the Intensive Care Unit for 24 hours for better monitoring. The total length of stay will depend on the degree of recovery. Subsequent drug therapy includes antiplatelet rather than anticoagulant drugs, unlike mechanical surgical valves.
Implantation of the new aortic valve immediately reduces symptoms to the extent that those were due to aortic stenosis, restores normal valve function and will improve overall heart function with increased life expectancy and quality of life. Both the American and European Heart Associations recommend non-surgical percutaneous valve implantation in high-risk patients or increased age (>75 years) as determined by a panel of cardiologists, cardiac surgeons and anesthesiologists.